Pneumonia
Highlights
Overview
- While the incidence of pneumonia is declining, it remains a widespread and significant health care issue in the U.S., particularly among people who need long-term medical care. An aging population, antibiotic resistance, and increasing health care costs make this a particularly challenging problem.
- Where an individual becomes infected with pneumonia is commonly used to describe a pneumonia case. Community-acquired pneumonia (CAP) is acquired in the community setting, not in a hospital or other care facility. Hospital (or nosocomial)-acquired pneumonia and nursing home-acquired pneumonia are acquired in those settings. Knowing the setting helps physicians predict which pathogens are most likely to be responsible for the infection.
- Pneumonia may have a viral or bacterial cause. Viral pneumonia accounts for a third or more of community-acquired pneumonias.
- Pneumonia symptoms vary among children, adults, and the elderly. Recognizing the symptoms of pneumonia promptly permits early diagnosis, appropriate antibiotic therapy, and a determination of where care should be delivered (such as ICU, hospital, or home). These steps contribute to positive outcomes.
- Doctors can use decision tools, such as the Pneumonia Severity Index (PSI), British Thoracic Society Rule (BSR), and the CURB-65, to determine the most appropriate level of care.
Risks
- Elderly adults, particularly those in nursing homes and those with other medical conditions, are at increased risk for pneumonia. Pneumonia is the second leading type of infection in nursing homes.
- Pneumonia is the most common hospital-acquired infection.
Treatment
- Ceftaroline, a cephalosporin, is newly approved for the treatment of community-acquired pneumonia and the first b-lactam active against methicillin-resistant Staphylococcus (S.) aureus (MRSA) and multidrug-resistant Streptococcus pneumoniae.
- Much research has been done on the duration of antibiotic therapy for pneumonia. Limiting exposure to antibiotic therapy where possible is generally preferred in order to minimize antibiotic resistance. In many cases, shorter courses of 7 - 8 days compared to the standard 10 - 15 days may be just as effective. Based on clinical response and laboratory results, certain patients may be treated with a shorter course of antibiotics (7 - 8 days). Recent evidence showed that even in certain cases of ventilator-associated pneumonia (VAP), shorter courses may be appropriate.
- Clinical re-evaluation within 24 - 48 hours of antibiotic treatment for CAP cases is prudent for children, adults, and the elderly.
Prevention
- The Centers for Disease Control and Prevention (CDC) Advisory Council recommends that all people ages 6 months and older, unless contraindicated, have a yearly flu shot. They are particularly important for seniors and other high risk individuals. Annual flu shots have been shown to reduce hospitalizations.
- The new pneumococcal conjugate vaccine series Prevnar 13 has replaced the older Prevnar 7. It is recommended for all children ages 6 weeks to 5 years.
- The pneumococcal polysaccharide vaccine is recommended for high risk individuals ages 2 - 65 and those over 65 years. A second dose is recommended 5 years after the initial dose in people who received their first dose before 65, and other high risk individuals. A conjugate vaccine for adults is nearing approval.
Introduction
Pneumonia is inflammation of the lung that is most often caused by infection with bacteria, viruses, or other organisms. Occasionally, inhaled chemicals can cause lung inflammation. Healthy people can usually fight off pneumonia infections. However, people who are sick, including those who are recovering from the flu (influenza) or an upper respiratory illness, have a weakened immune system. This makes it easier for bacteria to grow in their lungs. Pneumonia and influenza are the 8th leading cause of death in the U.S. Worldwide, pneumonia (with a bacterial origin) is the leading cause of death in children under age 5.
Defining Pneumonia by Location in the Lung
Pneumonia may be defined according to its location in the lung:
- Lobar pneumonia occurs in one part, or lobe, of the lung.
- Bronchopneumonia tends to be scattered throughout the lung.
Defining Pneumonia by Origin of Infection
Doctors often classify pneumonia based on where the disease is contracted. This helps predict which organisms are most likely responsible for the illness and, therefore, which treatment is most likely to be effective.
Community-Acquired Pneumonia (CAP). People with this type of pneumonia contracted the infection outside a hospital setting. It is one of the most common infectious diseases. It often follows a viral respiratory infection, such as the flu.
One of the most common causes of bacterial CAP is Streptococcus pneumoniae. Other causes include Haemophilus influenzae, Mycoplasma pneumoniae, and Chlamydia pneumoniae (which is not to be confused with a different chlamydia that is sexually transmitted).
Pneumonia Arising in an Institutional Setting
- Hospital-Acquired Pneumonia. Hospital-acquired pneumonia is an infection of the lungs contracted during a hospital stay. This type of pneumonia tends to be more serious because patients in the hospital already have weakened defense mechanisms, and the infecting organisms are usually more dangerous than those encountered in the community. Hospital patients are particularly vulnerable to Gram-negative bacteria and staphylococci. Hospital-acquired pneumonia is also called nosocomial pneumonia.
- Ventilator-associated pneumonia (VAP). A subgroup of hospital-acquired pneumonia is ventilator-associated pneumonia, a very serious infection contracted by patients on ventilators in hospitals and long-term nursing facilities.
- Nursing-home acquired pneumonia. Pneumonia acquired in a nursing home or other long-term care facility is the second most common type of infection in these facilities, usually bacterial. It is sometimes difficult to diagnose as older populations are less likely to report fever, chills, and chest pain. Chest radiography and physical exam are necessary. Sputum sample and antigen tests may be helpful.
Disease Process Leading to Pneumonia
Pneumonia-causing agents reach the lungs through different routes:
- In most cases, a person breathes in the infectious organism, which then travels through the airways to the lungs.
- Sometimes, the normally harmless bacteria in the mouth, or on items placed in the mouth, can enter the lungs. This usually happens if the body's "gag reflex," an extreme throat contraction that keeps substances out of the lungs, is not working properly.
- Infections can spread through the bloodstream from other organs to the lungs.
However, in normal situations, the airways protect the lungs from substances that can cause infection.
- The nose filters out large particles.
- If smaller particles pass through, nerves along the airway prompt a cough or sneeze. This forces many particles back out of the body.
- Tiny particles that reach the small tubes in the lungs (bronchioles) are trapped in a thick, sticky substance called mucus. The mucus and particles are pushed up and out of the lungs by tiny hair-like cells called cilia, which beat like a drum. This action is called the "mucociliary escalator."
- If bacteria or other infectious organisms manage to avoid the airway's defenses, the body's immune system attacks them. Large white blood cells called macrophages destroy the foreign particles.
The above-mentioned defense systems normally keep the lungs healthy. If these defenses are weakened or damaged, however, bacteria, viruses, fungi, and parasites can easily infect the lungs, producing pneumonia.
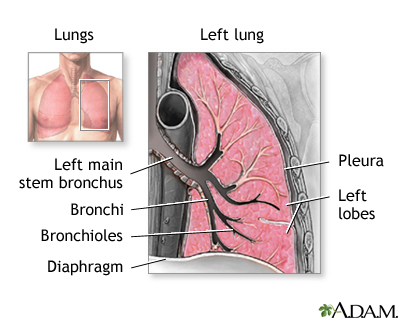
The Lungs
The lungs are two spongy organs in the chest surrounded by a thin, moist membrane called the pleura. Each lung is composed of smooth, shiny lobes. The right lung has three lobes, and the left has two. About 90% of the lung is filled with air. Only 10% is solid tissue. There are several parts to each lung.
When a person takes a breath (inhales), air travels from the windpipe (trachea) into the lung through the main bronchus, which branches into tiny flexible tubes called bronchi.
The bronchi divide, like the branches of a tree, into smaller airways called bronchioles.
The bronchioles lead to a group of microscopic sacs called alveoli, which look like clusters of grapes. Each healthy adult lung contains millions of tiny alveoli. (Note: The singular of alveoli is alveolus.)
Each alveolus has a thin membrane that allows oxygen and carbon dioxide to pass in and out of the capillaries, the smallest of the blood vessels. When you take a deep breath, the membrane unfolds and expands. Fresh oxygen moves into the capillaries, and carbon dioxide passes from the capillaries into the bloodstream, where it is carried out of the body through the lungs.
Blood vessels carry the oxygen-rich blood to the heart, where it is pumped throughout the body.
Causes
Bacteria are the most common causes of pneumonia. However, pneumonia can also be caused by viruses, fungi, and other agents. It is often impossible to identify the specific culprit.
Many bacteria are grouped into one of two large categories by the laboratory procedure used to look at them under a microscope. The procedure is known as Gram staining. Bacteria are stained with special dyes, then washed in a special solution. The color of the bacteria after washing determines whether they are Gram-negative or Gram-positive. Knowing which group the bacteria belong to helps determine the severity of the disease, and how to treat it. Different bacteria are treated with different drugs.
Gram-Positive Bacteria. These bacteria appear blue on the stain and are the most common organisms that cause pneumonia. They include:
- Streptococcus (S.) pneumoniae (also called pneumococcus), the most common cause of pneumonia. This Gram-positive bacterium causes 20 - 60% of all community-acquired bacterial pneumonia (CAP) in adults. Studies also suggest it causes 13 - 38% of CAP in children.
- Staphylococcus (S.) aureus, the other major Gram-positive bacterium responsible for pneumonia, causes about 2% of CAP and 10 - 15% of hospital-acquired pneumonias. It is the organism most often associated with viral influenza. It can develop about 5 days after the start of flu symptoms. Pneumonia from S. aureus most often occurs in people with weakened immune systems, very young children, hospitalized patients, and drug abusers who use needles. It is uncommon in healthy adults.
- Other Gram-positive bacteria that can sometimes cause pneumonia include Streptococcus pyrogenes (Group A streptococcus), and anerobic streptococci.
Gram-Negative Bacteria. These bacteria stain pink. Gram-negative bacteria commonly cause infections in hospitalized or nursing home patients, children with cystic fibrosis, and people with chronic lung conditions.
- Haemophilus (H.) influenzae is a bacterium. Despite its name, it is not related to the flu virus. H. influenzae is the second most common bacterium causing community-acquired pneumonia, accounting for 3 - 10% of all cases. It generally occurs in patients with chronic lung disease and older people.
- Klebsiella (K.) pneumoniae may be responsible for pneumonia in alcoholics and other people who are physically debilitated. It is also associated with recent use of very strong antibiotics.
- Pseudomonas (P.) aeruginosa is a major cause of hospital-acquired pneumonia (nosocomial pneumonia). It is a common cause of pneumonia in patients with chronic or severe lung disease.
- Moraxella (M.) catarrhalis is found in everyone's nose and mouth. Experts have identified this bacterium as an uncommon cause of certain pneumonias, particularly in people with lung problems such as asthma or emphysema.
- Other Gram-negative bacteria that cause pneumonia include E. coli, proteus (found in damaged lung tissue), enterobacter, Neisseria (N.) meningitidis, and acetinobacter.
Atypical Pneumonia
Atypical pneumonias produce mild symptoms and a dry cough. "Mini-epidemics" are sometimes seen in school or military settings. It occurs at any age, but it is more common in children and young adults. Organisms that cause atypical pneumonias include:
- Mycoplasma (M.) pneumoniae, the most common atypical pneumonia organism. Mycoplasma is a very small bacterium that lacks a cell wall. Pneumonia caused by M. pneumoniae spreads when someone carrying the infection comes in close contact with others for a long period of time. It is most often found in school-aged children and young adults. The condition, commonly called "walking pneumonia," is usually mild and seen in the outpatient setting.
- Chlamydia (C.) pneumoniae is now thought to cause 10% of all CAP cases. This atypical pneumonia is most common in young adults and children, and is usually mild. It is less common, but usually more severe, in the elderly.
- Legionella pneumophila causes Legionnaires' disease, a severe illness. It is contracted by breathing in drops of contaminated water. Outbreaks are often reported in hotels, cruise ships, and office buildings, where people are exposed to contaminated droplets from cooling towers and evaporative condensers. They have also been reported in people who have been near whirlpools and saunas. Legionella pneumophila is not passed from person to person. Some experts believe the organism causes up to 4% of all pneumonia cases.
Viral Pneumonia
Viral pneumonia accounts for a third or more of community-acquired pneumonia (CAP) cases. In young children, viral pathogens cause the majority of community-acquired pneumonia cases. Many viruses can cause pneumonia, either directly or indirectly. They include:
- Influenza (Flu). Pneumonia is a major complication of the flu (including H1N1, or swine flu) and can be very serious. Influenza-associated pneumonia is particularly risky for the elderly and people with heart disease. It can develop about 5 days after flu symptoms start. The flu weakens the body's defense systems, making it easier for bacteria to grow in the lungs.
- Respiratory syncytial virus (RSV). Most infants are infected with RSV at some point, but it is most often mild. However, RSV is a major cause of pneumonia in infants, as well as in adults with damaged immune systems. Studies indicate that RSV pneumonia may be more common in adults, especially the elderly, than previously thought.
- Human parainfluenza virus. This virus is a leading cause of pneumonia and bronchitis in children, the elderly, and patients with damaged immune systems.
- Adenoviruses. Adenoviruses are common and usually are not problematic, although they have been linked to about 10% of childhood pneumonias. Adenovirus 14 has been linked to an outbreak of severe community-acquired pneumonia in the Pacific Northwest as well as military recruits.
- Herpes viruses. In adults, herpes simplex virus and varicella zoster (the cause of chicken pox) can cause pneumonia in people with impaired immune systems.
- Avian influenza. Type A influenza subtype H5N1 in birds is spreading around the globe. Fortunately, only a few hundred human cases have been identified. Most have resulted from close contact with infected birds. The virus does not seem to spread easily from person to person. All patients diagnosed with "bird flu" show signs of pneumonia, although symptoms may be mild. Oseltamivir (Tamiflu) is the most effective treatment for this type of influenza, which can be fatal.
- Severe acute respiratory syndrome (SARS). SARS is a respiratory infection caused by a coronavirus, which appears to have jumped from animals to humans. The disease was first reported in China in 2003 but has not been a problem in recent years.
Though less common, many other viruses, bacteria, fungi, parasites, and infections can give rise to pneumonia.
Aspiration Pneumonia and Anaerobic Bacteria
The mouth contains a mixture of bacteria that is normally harmless. However, if this mixture reaches the lungs, it can cause a serious condition called aspiration pneumonia. This may happen after a head injury or general anesthesia, or when a patient takes drugs or alcohol. In such cases, the gag reflex doesn't work as well as it should, so bacteria can enter the airways. Unlike other organisms that are inhaled, bacteria that cause aspiration pneumonia do not need oxygen to live. These bacteria are called anaerobic bacteria.
Opportunistic Pneumonia
Impaired immunity leaves patients vulnerable to serious, life-threatening pneumonias known as opportunistic pneumonias. They are caused by organisms that are harmless to people with healthy immune systems. Infecting organisms include:
- Pneumocystis jiroveci (formerly called Pneumocystis carinii) is an atypical organism. Originally thought to be protozoa, it is now classified as a fungus. P. jiroveci is usually harmless in people with healthy immune systems. It is the most common cause of pneumonia in AIDS patients.
- Mycobacteria avium complex
- Viruses, such as cytomegalovirus (CMV)
- Fungi, such as Candida albicans
In addition to AIDS, other conditions put patients at risk for opportunistic pneumonia. They include cancers, such as lymphoma and leukemia. Long-term use of corticosteroids and drugs known as immunosuppressants also increases the risk for these pneumonias.
Occupational and Regional Pneumonias
Exposure to chemicals can also cause inflammation and pneumonia. Where you work and live can put you at higher risk for exposure to pneumonia-causing organisms.
- Workers exposed to cattle, pigs, sheep, and horses are at risk for pneumonia caused by anthrax, brucella, and Coxiella burnetii (which causes Q fever).
- Agricultural and construction workers in the Southwest are at risk for coccidoidomycosis (Valley fever). The disease is caused by the spores of the fungus Coccidioides immitis.
- Those working in Ohio and the Mississippi Valley are at risk for histoplasmosis, a lung disease caused by the fungus Histoplasma capsulatum.
- Workers exposed to pigeons, parrots, parakeets, and turkeys are at risk for psittacosis, a lung disease caused by the bacteria Chlamydia psittaci.
- Hantavirus, a rare virus carried by rodents, causes a dangerous form of lung disease. It does not spread from person to person. Cases have occurred in New Mexico, Arizona, California, Washington, and Mexico.
Symptoms
General Symptoms. Symptoms vary among children, adults, and the elderly. The symptoms of some bacterial pneumonias, such as pneumococcal pneumonia, develop very quickly and typically include:
- A single episode of shaking chills followed by fever
- Chest pain on the side of the infected lung. Severe abdominal pain sometimes occurs in people with pneumonia in the lower lobes of the lung
- Cough, which may be dry at first, but eventually produces phlegm (sputum)
- Night sweats
- Nausea, vomiting, and muscle aches
- Rapid breathing and heartbeat
- Shortness of breath
- Weight loss
Emergency Symptoms. Symptoms of pneumonia indicating a medical emergency include:
- Blood in sputum
- Bluish-toned (cyanotic) skin
- High fever
- Labored and heavy breathing
- Mental confusion or reduced mental function in the elderly
- Rapid heart rate
- Weight loss
Symptoms in Children. Common symptoms in infants include fever, rapid breathing, nasal flaring, and low oxygen saturation. Children ages 2 - 4 with pneumonia usually present with a cough plus one or more lower respiratory tract infection symptoms, such as fever, rapid breathing and low oxygen levels.
Symptoms in the Elderly. It is important to note that older people may have fewer or different symptoms than younger people. Symptoms may be subtle or non-specific. Some older people may be confused, lethargic, and show general deterioration.
Symptoms of Atypical Pneumonia
General Symptoms of Atypical Pneumonias. Atypical pneumonia is most commonly caused by mycoplasma, chlamydia, or a virus. It usually appears in children and young adults. Symptoms are usually mild and often go undiagnosed and untreated. Legionnaire's disease, however, is a severe form of atypical pneumonia that usually strikes adults and seniors.
The disease progresses gradually:
- General flu-like symptoms often occur first. They may include fatigue, fever, weakness, headache, nasal discharge, sore throat, earache, and stomach and intestinal distress.
- Vague pain under and around the breastbone may occur, but the severe chest pain associated with typical bacterial pneumonia is uncommon.
- Patients may have a severe hacking cough, but it usually does not produce sputum.
Prognosis
Between 5 and 10 million people get pneumonia in the United States each year. More than 1 million people are hospitalized due to the condition. As a result, pneumonia is the fourth most frequent cause of hospitalizations.
Although the majority of pneumonias respond well to treatment, the infection kills 40,000 - 70,000 people each year.
Men with community-acquired pneumonia tend to fare worse than women. Researchers say there may be some genetic reason for the disparity.
Outlook for High-Risk Individuals
Hospitalized Patients. The death rate for community-acquired pneumonia can range from well below 5% in mildly ill outpatients to 10 - 30% in seriously ill patients who need to be admitted to a hospital. If pneumonia develops in patients already hospitalized for other conditions, or those in a nursing home, death rates can be much higher. This is especially true for anyone who is on a ventilator.
Older Adults. Community-acquired pneumonia is responsible for 350,000 - 620,000 hospitalizations in the elderly every year. Older adults have lower survival rates than younger people. Even when older individuals recover from CAP, they have higher-than-normal death rates over the next several years. Elderly people who live in nursing homes or who are already sick are at particular risk.
Very Young Children. Small children who develop pneumonia and survive are at risk for developing lung problems in adulthood, including chronic obstructive pulmonary disease (COPD). Research suggests that men with a history of pneumonia and other respiratory illnesses in childhood are more than twice as likely to die of COPD as those without a history of childhood respiratory disease.
Pregnant Women. Pneumonia poses a special hazard for pregnant women, possibly due to changes in a pregnant woman's immune system. This complication can lead to premature labor and increases the risk of death during pregnancy.
Patients With An Impaired Immune System. Pneumonia is particularly serious in people with an impaired immune system. This is especially true for AIDS patients, in whom pneumonia causes about half of all deaths.
Patients With Serious Medical Conditions. Pneumonia is also very dangerous in people with diabetes, cirrhosis, sickle cell disease, cancer, and in those whose spleen has been removed.
Risk by Organisms
Specific organisms vary in their effects. Mild pneumonia is usually associated with the atypical organisms mycoplasma and chlamydia. Severe pneumonia is most often associated with a wide range of organisms. Some are very potent (virulent) but extremely curable, while others are difficult to treat:
- Mycoplasma and chlamydia are the most common causes of mild pneumonias and are most likely to occur in children and young adults. These patients rarely need hospitalization when they are appropriately treated, although recovery may still take time. Severe and life-threatening cases of pneumonia are more likely to occur in elderly people with other medical conditions.
- Streptococcus pneumoniae is the most common cause of pneumonia, as well as other bacterial upper respiratory infections. It can produce severe pneumonia, with mortality rates of 10%. Nevertheless, pneumococcal pneumonia responds very well to many antibiotics. Vaccination protects against several types of pneumococcal pneumonia.
- Staphylococcus aureus is a Gram-positive bacterium that often causes severe pneumonia in hospitalized and high-risk patients and following influenza A and B. People who get this form of pneumonia may develop pockets of infection in their lungs (abscesses) that are difficult to treat and can cause the death of lung tissue (necrosis). Mortality rates are 30 - 40%, in part because the patients who develop this infection are generally very ill or vulnerable.
- Pseudomonas aeruginosa and Klebsiella pneumoniae are Gram-negative bacteria that pose a risk for abscesses and severe lung tissue damage.
- Legionella pneumophila can spread easily from contaminated water droplets that enter the air. Treatments have improved dramatically since it was first identified. However, many patients may experience serious problems, including coughing, shortness of breath, fatigue, and nervous system (neurological) and muscle complications.
- Viral pneumonia is usually very mild, but there are exceptions. Respiratory syncytial virus (RSV) pneumonia rarely poses a danger for healthy young adults, but it can be life threatening in infants and serious in the elderly.
Complications of Pneumonia
Abscess. An abscess in the lung is a thick-walled, pus-filled cavity that forms when infection has destroyed lung tissue. It is more commonly seen with aspiration pneumonia, when a mixture of organisms is carried into the lung. Untreated abscesses can cause hemorrhage (bleeding) in the lung, but targeted antibiotic therapy significantly reduces the danger. Drainage with a needle may also be needed. Abscesses are more common with Staphylococcus aureus, Pseudomonas aeruginosa, or Klebsiella pneumoniae, and are uncommon with Streptococcus pneumoniae.
Respiratory Failure. Respiratory failure is one of the top causes of death in patients with more severe pneumonia. Acute respiratory distress syndrome (ARDS) is the specific condition that occurs when the lungs are unable to function and oxygen is so severely reduced that the patient's life is at risk. Failure can occur if pneumonia leads to physical changes in the lungs that make it even harder for the lungs to exchange oxygen (ventilatory failure).
Bacteremia. Bacteremia -- bacteria in the blood -- is the most common complication of pneumococcus infection, although it rarely spreads to other sites. Bacteremia is a frequent complication of infection from Gram-negative organisms, including Haemophilus influenzae.
Pleural Effusions and Empyema. The pleura is a two-layered membrane that surrounds each lung.
In some cases of pneumonia the pleura become inflamed, which can result in breathlessness and chest pain when breathing.
In about 20% of pneumonia cases fluid builds up between the pleural membranes, a condition known as pleural effusion. Ordinarily, the narrow zone between the two membranes contains only a tiny amount of fluid, which lubricates the lungs.
In most cases, particularly in Streptococcus pneumoniae, the fluid remains sterile (no bacteria are present), but occasionally it can become infected and even filled with pus, a condition called empyema. Empyema is more likely to occur with specific organisms, such as Staphylococcus aureus or Klebsiella pneumoniae infections. The condition can cause permanent scarring.
Collapsed Lung. In some cases, air may fill up the area between the pleural membranes, causing the lungs to collapse. This is called pneumothorax. It may be a complication of pneumonia (particularly Streptococcus pneumoniae) or of the invasive procedures used to treat pleural effusion.
Other Complications of Pneumonia. In rare cases, infection may spread from the lungs to the heart and possibly throughout the body. This can cause abscesses in the brain and other organs. At least one study has also linked bacterial pneumonia with an increased risk of acute heart problems, such as heart attack or abnormal heart rhythm (arrhythmia).
Kidney complications and electrolyte imbalances are common in patients admitted to the hospital with pneumonia. If not treated, these problems cause more severe illness and increase the risk of death. Hydration through a vein (intravenous) controls the problem.
Long-Term Effects of Atypical Pneumonias
Pneumonias cased by the atypical organisms mycoplasma and chlamydia are usually mild.
Asthma. Chlamydia pneumoniae, Mycoplasma pneumoniae, and RSV are becoming suspects in many cases of severe adult asthma. One small study found evidence of previous chlamydia infection in 64% of the patients with asthma who were tested.
Risk Factors
Risk factors for pneumonia often depend on the specific type of disease.
Risk Factors for Institutional- and Hospital-Acquired (Nosocomial) Pneumonia
Pneumonia that is contracted in the hospital is called hospital-acquired, or nosocomial, pneumonia. It is the most common hospital-acquired infection in the intensive care unit (ICU). It affects an estimated 5 - 10 of every 1,000 hospitalized patients every year. More than half of these cases may be due to strains of bacteria that have developed resistance to antibiotics. In fact, methicillin-resistant Staphylococcus aureus (MRSA) and multidrug-resistant Pseudomonas aeruginosa are leading causes of death from hospital-acquired pneumonia. Those at highest risk:
- The elderly and very young.
- People with chronic or severe medical conditions, such as lung problems, heart disease, nervous system (neurologic) disorders, and cancer.
- People who have had surgery, particularly people over age 80. Among the surgical procedures that pose a particular risk are removal of the spleen (splenectomy), abdominal aortic aneurysm repair, or operations that impair coughing.
- People who have been in the intensive care unit (ICU). This is particularly true for newborns or patients on breathing machines (mechanical ventilators). Patients who lie flat on their backs are at particular risk for aspiration pneumonia. Raising the patient up may reduce this risk.
- People who have received sedation. Hospital patients who receive sedatives also have a higher risk of developing nosocomial pneumonia.
- People who received antibiotics within previous 90 days.
Hospitalized patients are particularly vulnerable to Gram-negative bacteria and staphylococci, which can be especially dangerous in people who are already ill.
Risk Factors for Community-Acquired Pneumonia (CAP)
CAP is the most common type of pneumonia. It develops outside of the hospital. Each year 2 - 4 million people in the U.S. develop CAP, and 600,000 are hospitalized. The elderly, infants, and young children are at greatest risk for the disease.
Chronic Lung Disease. Chronic obstructive lung disease (COPD), which includes chronic bronchitis and emphysema, affects 15 million people in the U.S. This condition is a major risk factor for pneumonia. Long-term use of corticosteroid inhalers may increase the risk of pneumonia in COPD patients. Patients with other types of chronic lung diseases, such as bronchiectasis and interstitial lung diseases, are also at increased risk for getting pneumonia and more likely to have complications.
People With Compromised Immune Systems. People with impaired immune systems are extremely susceptible to pneumonia. It is a common problem in people with HIV and AIDS. A wide variety of organisms, including Pneumocystis jarovicil, myobacterium species, Histoplasma capsulatum, Coccidioides immitis, aspergillus species, cytomegalovirus, and Toxoplasma gondii, can cause pneumonia.
In addition to AIDS, other conditions that compromise the immune system include:
- Adult and pediatric cancers, especially leukemia and Hodgkin's lymphoma
- Chemotherapy
- Organ transplantation
Patients who are on corticosteroids or other medications that suppress the immune system are also prone to infection.
Also, drugs that treat gastroesophageal reflux (GERD) may slightly increase one's risk for community-acquired pneumonia. Patients at high risk for pneumonia should take gastric acid-suppressing drugs only when necessary and at the lowest possible dose. This association is strongest with protein pump inhibitors (PPIs) such as Prilosec and Nexium. Reducing levels of bacteria-killing stomach acid may allow germs to spread in the upper gastrointestinal tract and move into the respiratory tract. The risk posed by these medications is highest in:
- Children
- Patients with asthma, COPD, and compromised immune systems
- The elderly
Researchers have found that the risk is strongest when people have recently begun treatment with PPIs, and lessens over time.
Swallowing disorders, including dysphagia. Difficulty swallowing has a variety of causes, including:
- Abnormalities of the muscles of the esophagus
- Illnesses that affect swallowing, such as stroke, traumatic brain injury, or Parkinson's disease
- Surgery or radiation treatment for cancers of the mouth, throat, or esophagus
All of these may increase the risk of aspiration pneumonia.
Dementia. The lack of ability to concentrate while swallowing contributes to an increased risk of aspiration pneumonia. Elderly patients with dementia who are treated with antipsychotic drugs for psychosis have a 60% increased risk of developing pneumonia. Researchers are not sure why these drugs increase the pneumonia risk.
If a person inhales fluid (aspirates) from the esophagus into the lungs, it may trigger inflammation in these upper passages.
Factors Associated with a Higher Risk in Healthy Adults
Dormitory or Barrack Conditions. Recruits on military bases and college students living in dormitories are at higher-than-average risk for Mycoplasma pneumonia. These groups are at lower risk, however, for more serious types of pneumonia.
Smoke and Environmental Pollutants. The risk for pneumonia in people who smoke more than a pack a day is three times that of nonsmokers. Those who are chronically exposed to secondhand cigarette smoke, which can injure airways and damage the cilia, are also at risk. Quitting smoking reduces the risk of dying from pneumonia to normal, but the full benefit takes 10 years to be realized. Toxic fumes, industrial smoke, and other air pollutants may also damage cilia function, which is a defense against bacteria in the lungs.
Drug and Alcohol Abuse. Alcohol or drug abuse is strongly associated with pneumonia. These substances act as sedatives and can diminish the reflexes that trigger coughing and sneezing. Alcohol also interferes with the actions of macrophages, the white blood cells that destroy bacteria and other microbes. Intravenous drug abusers are at risk for pneumonia from infections that start at the injection site and spread through the bloodstream to the lungs.
Gender. Men with community-acquired pneumonia tend to fare worse than women. Men are 30% more likely than women to die from the condition. Researchers say there may be some genetic reason for the disparity.
Specific Risk Factors for Recurrent Pneumonia in Children
Certain children have a higher-than-normal risk for pneumonia and pneumonia that returns. Conditions that predispose infants and small children to pneumonia include:
- Abnormalities in muscle coordination of the mouth and throat
- Asthma
- Certain genetic disorders such as Kartagener syndrome, which result in poorly functioning cilia, the hair-like cells lining the airways
- Cystic fibrosis
- Bronchopulmonary dysplasia and other chronic lung diseases
- Prematurity, especially during the first 6 - 12 months of life
- Sickle cell disease
- Gastroesophageal reflux disorder (GERD)
- Impaired immune system
- Inborn lung or heart defects
Diagnosis
Diagnostic Difficulties in Community-Acquired Pneumonia (CAP). It is important to determine whether the cause of CAP is a bacterium, atypical bacterium, or virus, because they require different treatments. In children, for example, S. pneumoniae is the most common cause of pneumonia, but respiratory syncytial virus may also cause the disease. Although symptoms may differ, they often overlap, which can make it difficult to identify the organism by symptoms alone. The cause of CAP is found in only about half of cases.
Nevertheless, in many cases of mild-to-moderate CAP, the physician is able to diagnose and treat pneumonia based solely on a medical history and physical examination.
Diagnostic Difficulties with Hospital-Acquired (Nosocomial) Pneumonia. Diagnosing pneumonia is particularly difficult in hospitalized patients for a number of reasons:
- Many hospitalized patients have similar symptoms, including fever or abnormal x-rays.
- In hospitalized patients, sputum or blood tests often show bacteria or other organisms, but such agents do not necessarily indicate pneumonia.
Medical and Personal History
The patient's history is an important part of making a pneumonia diagnosis. Patients should report any of the following:
- Alcohol or drug abuse
- Exposure to people with pneumonia or other respiratory illnesses (such as tuberculosis)
- History of smoking
- Occupational risks
- Recent or chronic respiratory infection
- Recent antibiotic therapy
- Recent outpatient wound care
- Home infusion therapy or dialysis
- Recent travel
- Exposure to birds, bats, or other animals
Physical Examination
Use of the Stethoscope. The most important diagnostic tool for pneumonia is the stethoscope. Sounds in the chest that may indicate pneumonia include:
- Rales, a bubbling or crackling sound. Rales strongly suggest pneumonia.
- Rhonchi, abnormal rumblings indicating that there is sputum in the large airways.
- A dull thud. The physician will use a test called percussion, in which the chest is tapped lightly. A dull thud, instead of a hollow drum-like sound, indicates certain conditions that suggest pneumonia. These conditions include consolidation (in which the lung becomes filled with fluid and pus) and pleural effusion (fluid build-up in the space between the lungs and the lining around it).
Pulse Oximetry. A pulse oximetry test can help determine if a patient needs hospital care. A simple test using a device on the fingertip or earlobe, this determines the amount of oxygen in the blood.
Laboratory Tests for Diagnosing Infection and Identifying Bacteria
Although current antibiotics can attack a wide spectrum of organisms, it is best to use an antibiotic that targets the specific one making a person sick. Unfortunately, people carry many bacteria, and sputum and blood tests are not always effective in distinguishing between harmless and harmful kinds. The Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) recommends diagnostic testing when it may impact the choice of antibiotic and in patients with a high likelihood of accurate results (sicker patients). Many of these laboratory tests take 4 - 5 days or longer to complete, however, and therapy should be started before results are available.
Although viral pneumonia accounts for more than a third of community-acquired pneumonia cases, it can sometimes be difficult to determine if the pneumonia is viral or bacterial in origin.
In severe cases, a doctor needs to use invasive diagnostic measures to identify the cause of the infection. These tests are not commonly performed in outpatients. Standard lab tests are used to help diagnose pneumonia.
Sputum Tests. A sputum sample may reveal the organism causing the infection.
The patient coughs as deeply as possible to bring up mucus from the lungs, since a shallow cough produces a sample that usually only contains normal mouth bacteria. Some people may need to inhale a saline spray to produce an adequate sample. In some cases, a tube will be inserted through the nose into the lower respiratory tract to trigger a deeper cough.
The physician will check the sputum for:
- Blood, which suggests an infection is present.
- Color and consistency: If it is gray, green, or brown, an infection is likely.
The sputum sample is sent to the laboratory, where it is analyzed for the presence of bacteria and to determine whether the bacteria are Gram-negative or Gram-positive.
Blood Tests. The following blood tests may be performed:
- White blood cell count (WBC). High levels indicate infection.
- Blood cultures. Cultures are done to determine the specific organism causing the pneumonia, but they usually cannot distinguish between harmless and dangerous organisms. They are accurate in only 10 - 30% of cases. Their use is generally limited to severe cases.
- Detection of antibodies. Antibodies are immune factors that target specific foreign invaders. Antibodies that react with mycoplasma or chlamydia are not present early enough in the course of pneumonia to allow for prompt diagnosis by this method.
- C-reactive protein or procolacitonin. Not generally recommended but may help identify which patients with respiratory symptoms have pneumonia and need to be hospitalized.
- Polymerase Chain Reaction (PCR). In some difficult cases, PCR may be performed. The test makes multiple copies of the genetic material (RNA) of a virus or bacteria to make it detectable. PCR is useful for identifying certain atypical bacteria strains, including mycoplasma and Chlamydia pneumoniae, but it is expensive. One study found that using a real-time PCR test may help quickly diagnose Pneumocystitis pneumonia in HIV-positive patients.
Urine Tests. Urine antigen tests for Legionella pneumophila (Legionnaires' disease) and Streptococcus pneumoniae may be performed in patients with severe CAP. The S. pneumoniae test takes only 15 minutes and may identify up to 77% of pneumonia cases and rule out S. pneumoniae infection in 98% of patients. It may not be useful in children.
Invasive Tests. In critically-ill patients with ventilator-associated pneumonia, doctors have tried sampling fluid taken from the lungs or trachea. These techniques enabled the physicians to identify the pneumonia-causing bacteria and start the appropriate antibiotics. However, this made no difference in the length of stay in the ICU or hospital, and there was no significant difference in outcome.
Chest X-Rays and Other Imaging Techniques
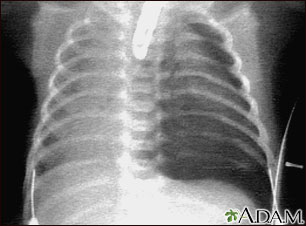
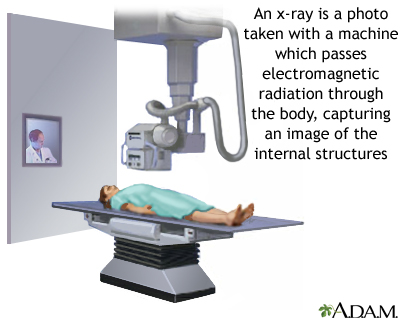
X-Rays. A chest x-ray is nearly always taken on a patient admitted to the hospital to confirm a pneumonia diagnosis. This does not need to be repeated if the patient gets better.
A chest x-ray may reveal the following:
- Complications of pneumonia, including pleural effusions and abscesses
- White areas in the lung called infiltrates, which indicate infection
Other Imaging Tests. Computed tomography (CT) scans or magnetic resonance imaging (MRI) scans may be useful in some circumstances, especially when:
- A lung tumor is suspected
- Complications occur
- Patients do not respond to antibiotics
- Patients have other serious health problems
- Pulmonary embolism is suspected
- X-ray results are unclear
CT and MRI can help detect tissue damage, abscesses, and enlarged lymph nodes. They can also detect some tumors that block bronchial tubes. No imaging technique can determine the actual organism causing the infection. However, features on the CT scan of patients with certain forms of pneumonia -- for example, that are caused by Legionella pneumophila -- are usually different from features produced by other bacteria in the lungs.
Invasive Diagnostic Procedures
Invasive diagnostic procedures may be necessary when:
- Patients have AIDS or other immune problems
- Patients have life-threatening complications
- Standard treatments have failed for no known reason
Thoracentesis. If a doctor detects pleural effusion during the physical exam or on an imaging study, and suspects that pus (empyema) is present, a thoracentesis is performed.
- Fluid in the pleura is withdrawn using a long thin needle inserted between the ribs.
- The fluid is then sent to the lab for multiple tests.
Complications of this procedure are rare, but they can include collapsed lung, bleeding, and infection.
Bronchoscopy. Bronchoscopy is an invasive test to examine respiratory secretions. It is not usually needed in patients with community-acquired pneumonia, but it may be appropriate for patients with a severely compromised immune system who need immediate diagnosis, or in patients whose condition has worsened during treatment.
A bronchoscopy is done in the following way:
- The patient is given a local anesthetic, oxygen, and sedatives.
- The physician inserts a fiber optic tube into the lower respiratory tract through the nose or mouth.
- The tube acts like a telescope into the body, allowing the physician to view the windpipe and major airways and look for pus, abnormal mucus, or other problems.
- The doctor removes specimens for analysis and can also treat the patient by removing any foreign bodies or infected tissue encountered during the process.
Bronchoalveolar lavage (BAL) may be done at the same time as bronchoscopy. This involves injecting high amounts of saline through the bronchoscope into the lung and then immediately sucking the fluid out. The fluid is then analyzed in the laboratory. Studies find BAL to be an effective method for detecting specific infection-causing organisms.
The procedure is usually very safe, but complications can occur. They include:
- Allergic reactions to the sedatives or anesthetics
- Asthma attacks in susceptible patients
- Bleeding
- Fever
Lung Biopsy. In very severe cases of pneumonia or when the diagnosis is unclear, particularly in patients with a damaged immune system, a lung biopsy may be required. A lung biopsy involves taking some tissue from the lungs and examining it under a microscope.
Lung Tap. This procedure typically uses a needle inserted between the ribs to draw fluid out of the lung for analysis. It is known by a number of names, including:
- Lung aspiration
- Lung puncture
- Thoracic puncture
- Transthoracic needle aspiration
- Percutaneous needle aspiration
- Needle aspiration
This is a very old procedure that is not done often anymore because it is invasive and poses a slight risk for collapsed lung. Some experts argue, however, that a lung tap is more accurate than other methods for identifying bacteria, and the risk it poses is slight. Given the increase in resistant bacteria, they believe its use should be reconsidered in young people.
An infectious disease specialist may need to be consulted in severe or difficult cases.
Ruling Out Other Disorders that Cause Coughing or Affect the Lung
Common Causes of Persistent Coughing. Persistent coughing is nearly always temporary and harmless when other symptoms, such as fever, are not present. The four most common causes of persistent coughing are:
- Asthma
- Chronic bronchitis
- Gastroesophageal reflux disease (GERD)
- Postnasal drip
Other common causes of chronic cough include heavy smoking or the use of blood pressure drugs known as ACE inhibitors.
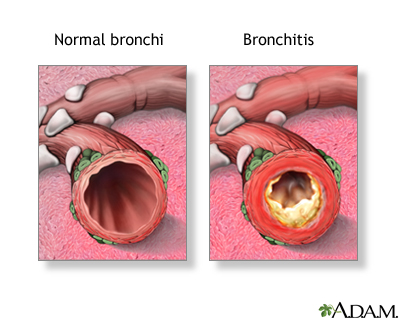
Acute Bronchitis. Acute bronchitis is an infection in the passages that carry air from the throat to the lung. The infection causes a cough that produces phlegm. Acute bronchitis is almost always caused by a virus and usually clears up on its own within a few days. In some cases, acute bronchitis caused by a cold can last for several weeks.
Chronic Bronchitis. Chronic bronchitis causes shortness of breath and is often accompanied by infection, mucus production, and coughing, but it is a long-term and irreversible condition. The same bacteria and viruses that cause pneumonia can cause an infection in patients with chronic bronchitis. However, infections involve only the airways leading to the lungs, and not the lung tissue itself. The two disorders may share the same symptoms, such as:
- Coughing
- Fatigue
- Fever
- Sputum production
There are significant differences between chronic bronchitis and pneumonia:
- Patients with bronchitis are less likely to have wheezing, shortness of breath, chills, very high fevers, and other signs of severe illness.
- Those with pneumonia often cough up heavy sputum, which may contain blood.
- X-rays of patients with pneumonia show inflammation and other changes in the lung tissue that are not seen in patients with chronic bronchitis.
Asthma. In asthma, the cough is usually accompanied by wheezing and occurs mostly at night or during activity. Fever is rarely present (unless the patient also has an infection). Asthma symptoms from occupational causes can lead to persistent coughing, which is usually worse during the work week. Tests -- the methacholine inhalation challenge and pulmonary function studies -- may be effective in diagnosing asthma.
Other Disorders that Affect the Lung. Many conditions mimic pneumonia, particularly in hospitalized patients. They include:
- Acute respiratory distress syndrome (ARDS)
- Atelectasis, a partial collapse of lung tissue
- Bronchiectasis, an irreversible widening of the airways that is usually associated with birth defects, chronic sinus or bronchial infection, or blockage
- Heart failure (if it affects the left side of the heart, fluid build-up can occur in the lungs and cause persistent cough, shortness of breath, and wheezing)
- Interstitial pulmonary fibrosis, a non-infectious inflammation of the lung that causes damage and scarring
- Lung cancer
- Severe allergic reactions, such as reactions to drugs
- Tuberculosis
Ruling Out Causes in Children. Important causes of coughing in children at different ages include:
- Asthma
- Sinusitis in children 18 months - 6 years
Treatment
The approach to treating patients with pneumonia generally involves:
- Deciding who can be treated at home and who needs to be in the hospital
- Deciding whether a patient needs antibiotics, and which antibiotics are appropriate
- Providing appropriate supportive care
- Deciding what follow-up and preventive care are needed
Whether patients are treated at home or admitted to the hospital, receiving their first dose of antibiotics quickly improves the outcome of the illness and the speed at which they get better.
Determining the Need for Hospitalization
Determining the site of care is an important clinical decision. A clinician must decide whether the patient would best be treated in one of the following settings:
- Outpatient
- Short term hospital stay or observational unit
- Inpatient
Studies indicate that many adult patients do not need to be hospitalized for pneumonia, and can be safely treated at home. Likewise, many patients who are admitted to the hospital could be released sooner. Many strategies are being devised to determine which patients can be safely discharged and when they can be discharged. In general, low-risk patients with mild-to-moderate pneumonia do just as well when treated as outpatients. They return to work and normal activities faster than those treated in the hospital.
A variety of guidelines and tools have been developed to help determine who can safely be treated at home and who cannot. Commonly used tools include the Pneumonia Severity Index (PSI), British Thoracic Society Rule (BSR), and CURB-65. All of these assessment tools evaluate several risk factors. The more of these risk factors that are present, the less likely that the patient can be safely treated at home. The combination of these risk factors determine a specific score or risk group, helping to guide the clinician in the decision. The results must be used along with the doctor's clinical judgment.
Some of the important factors used to make a decision include:
Demographics.
- Patients who have been living in a nursing home or other residential facility are of greater concern.
- Elderly patients and infants, particularly infants younger than 1 month old, are more likely to be admitted.
Other Medical Illnesses. Patients may be considered at greater risk if they have:
- Cancer
- Heart failure
- History of stroke
- Kidney failure
- Liver disease
Findings on a Physical Exam. Concerning findings include:
- Altered mental status (confused, less responsive)
- Appearance of being dehydrated, especially if the person is unable to drink fluids
- Fast breathing (more than 30 breaths per minute)
- Heart rate greater than 120 beats per minute
- Systolic blood pressure less than 90 mmHg
- Temperature greater than 104 °F
Laboratory and X-ray Findings. Laboratory findings that are of concern include:
- Elevated blood sugar
- Fluid in the pleural space around the lung (on chest x-ray)
- Low oxygen in the blood
- Low sodium levels
- Poor kidney function
- Significant anemia (hematocrit less than 30%)
Patients with very few of these risks often can be discharged with outpatient care only. This determination can often be made with a simple physical examination and history. Sometimes a patient needs to be hospitalized for only 24 hours for observation.
Patients with higher scores on these assessment tests often have many risk factors and usually are hospitalized.
When possible, treatment of community-acquired pneumonia should be started within 4 hours of admission to the emergency room or hospital to reduce the chances of mortality and decrease the amount of time a patient needs to spend in the hospital.
The following characteristics should prompt hospitalization in children and infants:
- Children and infants with severe community acquired pneumonia, such as those having great difficulty breathing and with low levels of oxygen in the blood (SpO2<90%)
- Infants less than 3-6 months of age with suspected bacterial community-acquired pneumonia
- Children and infants with suspected community-acquired pneumonia caused by a bacteria or virus known to cause serious illness, such as methicillin-resistant Staphylococcus aureus (CA-MRSA)
- Children and infants for whom proper care at home or follow-up is a concern
Home care may be possible, even in severe cases, when there is good support and available home nursing services. Often, caregivers can even be trained to administer intravenous antibiotics and chest therapy to patients at home.
Home Treatment
The following tips are suggested:
- Drink plenty of liquids (1 - 2 quarts daily).
- Take oral temperature several times a day. Call your doctor if it does not come down with treatment.
- Do not suppress a cough. Coughing is an important reflex for clearing the lungs. Some doctors advise taking expectorants, such as guaifenesin (Breonesin, Glycotuss, Glytuss, Hytuss, Naldecon Senior EX, Robitussin) to loosen mucus. However, there is no proof that any of these products make much difference in a patient's outcome.
- Mild pain can be treated with aspirin (in adults only), acetaminophen (Tylenol), or ibuprofen (Advil, Motrin).
- For severe pain, codeine or another stronger pain reliever may be prescribed. It should be noted, however, that codeine and other narcotics suppress coughing, so they should be used with care in pneumonia. Such pain relievers often require monitoring.
- Finish entire course of antibiotics.
- Don't smoke.
Hospitalization Guidelines
Treatment. If the pneumonia is severe enough for hospitalization, the standard treatment is intravenous antibiotics for 5 - 8 days. In cases of uncomplicated pneumonia, many patients may need only 2 or 3 days of intravenous antibiotics followed by oral therapy. Antibiotics taken by mouth are prescribed when the patient has improved substantially or leaves the hospital.
ITSA/ATS guidelines recommend that patients admitted to the hospital (but not the ICU) be treated with fluoroquinolones or a beta-lactam (preferably cefotaxime or ceftriaxone) plus a macrolide.
Duration of Stay. Patients should remain in the hospital until all their vital signs are stable. Most patients become stabilized in 3 days and can continue treatment at home. Many experts use seven variables to measure stability and to determine whether the patient can go home:
- Temperature. Some experts believe that patients can go home when their temperature drops to 101 °F. Stricter criteria require that it be at or close to 98.6 °F.
- Respiration rate. The goal is a normal breathing rate, although expert opinion differs on the degree of normality required for discharge.
- Heart rate. The goal is 100 beats per minute or less.
- Blood pressure. The goal is systolic blood pressure of 90 mmHg or greater.
- Oxygenation. The doctor determines the goal.
- The ability to eat. The goal is regular appetite.
- Mental function. The goal is normal.
Patients or their families should discuss these criteria with their doctor.
Chest Therapy
Chest therapy using incentive spirometry, rhythmic inhalation and coughing, and chest tapping are all important techniques to loosen the mucus and move it out of the lungs. It should be used both in the hospital and during recovery at home.
Incentive Spirometry. The patient uses an incentive spirometer at regular intervals to improve breathing and loosen sputum. The spirometer is a hand-held clear plastic device that includes a breathing tube and a container with a movable gauge. The patient exhales, then inhales forcefully through the tube, using the pressure of the inhalation to raise the gauge to the highest level possible.
Rhythmic Breathing and Coughing. During recovery, the patient performs rhythmic breathing and coughing every 4 hours:
- Before starting the breathing exercise, the patient should tap lightly on the chest to loosen mucus in the lung. If available, a caregiver should also tap on the patient's back.
- The patient inhales rhythmically and deeply three or four times.
- The patient then coughs as deeply as possible with the goal of producing sputum.
Oxygen Therapy
Patients who are not able to get enough oxygen into their cells and bloodstream may need oxygen therapy. It may be done in the hospital or at home under medical supervision. Delivery systems include an oxygen concentrator or more mobile cylinder option. Nasal prongs or a face mask will deliver the oxygen. Oxygen levels will be monitored regularly. Anyone using oxygen should stay away from open flames, including cigarettes.
Medications
Dozens of antibiotics are available for treating pneumonia, but selecting the best drug is sometimes difficult. Patients with pneumonia need an antibiotic that is effective against the organism causing the disease. When the organism is unknown, "empiric therapy" is given, meaning the doctor chooses which antibiotic is likely to work based on factors such as the patient's age, health, and severity of the illness.
In adults, the choice of antibiotic therapy depends on the severity of infection and site of care. In all cases, the more quickly antibiotic therapy is started once the diagnosis is made, the better the outcomes. In most cases, the organism causing the pneumonia will not be known before antibiotic therapy is started, so the doctor must choose an antibiotic regimen based on history and symptoms. Later, the therapy may be altered when more information becomes available. To determine the appropriate antibiotic, the doctor must first answer a number of questions:
- How severe is the pneumonia? Patients with mild-to-moderate cases take oral antibiotics at home. Patients with severe pneumonia usually need intravenous antibiotics in the hospital.
- If the organism causing the pneumonia is not known, was the disorder community- or hospital-acquired? Different organisms are usually involved in each setting. The doctor can use this information to guess the most likely organism causing the pneumonia.
- If the organism is known, is it typical or atypical? Community-acquired pneumonias, for example, are usually caused by the typical bacteria Streptococcus pneumoniae, Haemophilus influenzae, or Moraxella catarrhalis, which were previously treated with related antibiotics. These antibiotics do not treat organisms such as legionella, mycoplasma, or chlamydia. These organisms are generally treated with a macrolide or a newer fluoroquinolone.
- Does the patient have an impaired immune system? Antibiotics used to treat such patients may differ from those used in patients with healthy immune systems.
Once an antibiotic has been chosen, there are still difficulties:
- Individuals respond differently to the same antibiotic, depending on their age, health, size, and other factors.
- Patients can be allergic to certain antibiotics, thus requiring alternatives.
- Patients may have strains of bacteria that are resistant to certain antibiotics.
Antibiotic Treatments for Community-Acquired Pneumonia
Joint guidelines issued in 2007 by the Infectious Disease Society of America and the American Thoracic Society (ITSA/ATS) recommend that mild CAP in otherwise healthy patients be treated with an oral macrolide antibiotic (such as azithromycin or clarithromycin).
The British Thoracic Society recommends amoxicillin, doxycycline, or clarithromycin as alternatives.
Many patients with heart disease, kidney disease, diabetes, or other co-existing conditions may still be treated as outpatients. Those without recent antibiotic use should be given a fluoroquinolone (moxifloxacin, gemifloxacin, or
levofloxacin) or a macrolidesuch asazithromycinor clarithromycin (unless they live in an area with high S. pneumoniae resistance to macrolides).
Patients with co-existing conditions that have taken antibiotics recently should be given a macrolide plus high-dose
amoxicillin, amoxicillin/clavulanate, cefpodoxime, cefprozil, or cefuroxime or a fluoroquinolone. Many patients with heart disease, kidney disease, diabetes, or other co-existing conditions may still be treated as outpatients. However, they should be given a fluoroquinolone (moxifloxacin, gemifloxacin, or levofloxacin) or a beta-lactam (preferably high-dose amoxicillin or amoxicillin-clavulanate), plus a macrolide, unless they live in an area with high S. pneumoniae resistance to macrolides.
Current recommendations call for 7 - 10 days of treatment for S. pneumoniae and 10 - 14 days for Mycoplasma pneumoniae and Chlamydia pneumoniae. However, the efficacy of antibiotics in children with M. pneumonia is unclear, and quite often "walking pneumonia" goes undiagnosed and untreated. In addition, some research suggests that patients with mild-to-moderate community-acquired pneumonia may be successfully treated with 7 days or less of antibiotics. The shorter treatment may increase patient tolerance, and improve the likelihood that patients will stick to the treatment regimen. It will also help limit the growing problem of antibiotic resistance.
For a more detailed discussion of the different types of antibiotics, see the "Antibiotic Classes" section below.
Many cases of community-acquired pneumonia are caused by S. pneumoniae -- Gram-positive bacteria that usually respond to antibiotics known as beta-lactams (which include penicillin), and to macrolides. However, resistant strains of S. pneumoniae are increasingly common. Most resistant strains respond to fluoroquinolines such as levofloxacin (Levaquin), gemifloxacin (Factive), or moxifloxacin (Avelox). Another common cause of community-acquired pneumonia is H. influenzae.
In addition, other important causes of CAP, particularly in younger people, are atypical bacteria, which respond to macrolides (clarithromycin or azithromycin), or newer fluoroquinolones. A review of research in children under 18 years of age has indicated amoxicillin, co-trimaxazole, co-amoxyclavulanic acid, and cefpodoxime as options in the ambulatory child with pneumonia. As well, oral amoxicillin may be an alternative to injectable penicillin in the hospitalized child.
Antibiotic treatment for CAP is determined by several factors, including:
- The patient's history of antibiotic therapy
- Co-existing diseases (such as COPD, diabetes, and heart failure)
- Whether the patient is well enough to be treated at home or requires hospitalization or nursing home care.
Treatment options can include a single drug, such as levofloxacin or doxycycline, or combination treatment, such as a macrolide administered with a beta-lactam.
Antibiotics taken by mouth are generally enough for patients whose CAP is mild enough to be treated at home. Intravenous antibiotics are required for hospitalized patients with CAP. Antibiotic therapy should be given for a minimum of 5 days -- longer if the patient still has a fever and more than one sign of continuing severe illness.
In children, amoxicillin is the first line treatment in non-severe pneumonia. Macrolides may be considered for children with suspected atypical pathogens. Antiviral medications should be given to children with moderate to severe community-acquired pneumonia with influenza infection as soon as possible.
It is prudent to follow up on outpatient treatment response within 48 - 72 hours of initiating treatment.
Antibiotic Treatments for Hospital-Acquired (Nosocomial) Pneumonia
A broad range of antibiotics is available for treating hospital-acquired pneumonias and more severe forms of the condition. Factors that may determine the choice of an antibiotic include:
- Immune status
- Patterns of antibiotic resistance within a particular hospital or community
- Recent antibiotic usage
- Type of bacteria causing the pneumonia
- Use of ventilators
Many studies are assessing the duration of antibiotic treatment, and when it is save to reduce the length of the course of antibiotics.
Treatment of Viral Infections
There are not as many choices for treating viral pneumonia. Oseltamivir (Tamiflu) and zanamivir (Relenza) have been the recommended drugs for influenza A or B infections, but some strains of influenza A are resistant. Generally, their use is only recommended if they are started in the first 48 hours of symptoms. Taken early, these medications may be effective in reducing symptoms and duration of illness. However, treatment initiated after 48 hours may benefit children with severe disease.
Patients with viral pneumonias are at risk for what are called "superinfections," which generally refers to a secondary bacterial infection, usually caused by S. pneumoniae, S. aureus, or H. influenzae. Doctors most commonly recommend treatment with amoxicillin-clavulanate, cefpodoxime, cefprozil, cefuroxime, or a newer fluoroquinolone if these secondary infections occur.
Patients with pneumonia caused by varicella-zoster and herpes simplex viruses are usually admitted to the hospital and treated with intravenous acyclovir for 7 days.
No antiviral drugs have been proven effective in adults with RSV, parainfluenza virus, adenovirus, metapneumovirus, the SARS coronavirus, or hantavirus. Treatment is largely supportive, with patients receiving oxygen and ventilator therapy as needed.
Treatment of RSV in Children. Ribavarin is the first treatment approved for RSV pneumonia, although it has only modest benefits. The American Academy of Pediatrics recommends this drug for certain children who are at high risk for serious complications of RSV.
Side Effects of Antibiotics
Most antibiotics have the following side effects (although specific antibiotics may have other side effects or fewer of the standard ones):
- Allergic reactions (most commonly with medications derived from penicillin or sulfa). These reactions can range from mild skin rashes to rare but severe -- even life-threatening -- anaphylactic shock.
- Infection with Clostridium difficile, the bacteria responsible for causing severe diarrhea, inflammation of the colon (colitis), and abdominal pain (with overuse of antibiotics). This condition can be fatal.
- Interactions with certain drugs, including some over-the-counter (OTC) medications and supplements. Patients should inform their doctors of all medications and OTC preparations they are taking, as well as any drug allergies they might have.
- Stomach problems (most common side effect).
- Vaginal infections. Taking acidophilus supplements or eating yogurt with active acidophilius cultures may help restore healthy bacteria that reduce the risk for such infections.
Antibiotic and Antiviral Drug Classes
Beta-Lactams
Beta-lactam antibiotics share common chemical features. They include penicillins, cephalosporins, and some newer similar medications. They interfere with bacterial cell walls.
Penicillins. Penicillin was the first antibiotic. There are many forms of this still-important drug:
- Natural penicillins include penicillin G (for intravenous use) and V (for oral use).
- Penicillin derivatives called aminopenicillins, particularly amoxicillin (Amoxil, Polymox, Trimox, Wymox, or any generic formulation), are now the most common penicillins used. Amoxicillin is inexpensive and, at one time, was highly effective against S. pneumoniae. Unfortunately, bacterial resistance to amoxicillin has increased significantly, both among S. pneumoniae and H. influenzae. Ampicillin is similar and is an alternative to amoxicillin, but it requires more doses and has more gastrointestinal side effects.
- Amoxicillin-clavulanate (Augmentin) is a type of penicillin that works against a wide variety of bacteria. An extended-release form has been approved for treating adults with community-acquired pneumonia caused by bacterial strains that have become partially resistant to penicillin.
- Antistaphylococcal penicillins were developed to treat Staphylococcus aureus. The standard drug was methicillin; it has been replaced by related drugs, but they are no longer used routinely, due to very high rates of resistance in hospital-acquired pneumonias. Resistance in community-acquired Staphylococcus aureus is also increasing. Alternatives include vancomycin, linezolid, daptomycin, and ceftaroline, the first b-lactam drug that is active against methicillin-resistant Staph. aureus.
- Penicillins used against Pseudomonas aeruginosa include ticarcillin and piperacillin. Piperacillin is more effective than ticarcillin.
Many people have a history of an allergic reaction to penicillin, but research suggests that the allergy may not occur again in a significant number of adults. Skin tests are available to help determine if those with a history of penicillin allergies could use these important antibiotics.
Cephalosporins. Most of these antibiotics are not very effective against bacteria that have developed resistance to penicillin. They are classed according to their generation:
- First generation includes cephalexin (Keflex), cefadroxil (Duricef, Ultracef), and cephradine (Velosef).
- Second generation includes cefaclor (Ceclor), cefuroxime (Ceftin), cefprozil (Cefzil), and loracarbef (Lorabid).
- Third generation includes cefpodoxime (Vantin), cefdinir (Omnicef) cefditoren (Sprectracef), cefixime (Suprax), and ceftibuten (Cedex). Ceftriaxone (Rocephin) is an injected cephalosporin. These are effective against a wide range of Gram-negative bacteria.
Other Beta-Lactam Agents. Ceftaroline, a cephalosporin, is newly approved and the first b-lactam active against methicillin-resistant Staphylococcus aureus (MRSA) and multidrug-resistant Streptococcus pneumoniae.
Carbapenems include meropenem (Merrem), ertapenem (Invanz) and combinations [imipenem/cilastatin (Primaxin)]. These drugs are used to treat a wide variety of bacteria. They are now used for serious hospital-acquired infections and bacteria that have become resistant to other beta-lactams.
Sanfetrinem, a new beta-lactam antibiotic known as a trinem, is proving to be effective against S. pneumoniae, H. influenzae, and M. catarrhalis.
Ceftobiprole is an investigational beta-lactam for methicillin-resistant Staphylococcus aureus (MRSA), penicillin-resistant streptococci, and other Gram-negative bacteria. Another anti-MRSA beta-lactam in development is CS-023/RO-4908463, a carbapenem.
Fluoroquinolones
Fluoroquinolones (quinolones) interfere with bacteria's genetic material to prevent them from reproducing.
- Ciprofloxacin (Cipro), a second-generation quinolone, remains the most potent quinolone against Pseudomonas aeruginosa. It is not very effective against Gram-positive bacteria such as Streptococcus pneumoniae.
- Newer ("respiratory") quinolones are currently the most effective drugs available for a wide range of bacteria. Such drugs include levofloxacin (Levaquin) and gemifloxacin (Factive). Some of the newer fluoroquinolones need to be taken only once a day.
- The fourth-generation quinolones moxifloxacin (Avelox) and clinafloxacin (which is still under development) are proving to be effective against anaerobic bacteria.
S. pneumoniae -- strains resistant to the "respiratory" fluoroquinolones are uncommon in the U.S., but resistance is dramatically increasing.
Many quinolones cause side effects, including:
- Nervous system, mental, and heart problems
- Sensitivity to light
Pregnant women should not take these medications. The drugs also enhance the potency of oral anti-clotting drugs.
Macrolides
Macrolides also affect the genetics of bacteria. These medications include:
- Azithromycin (Zithromax, Zmax)
- Clarithromycin (Biaxin)
- Erythromycin
- Roxithromycin (Rulid)
These antibiotics are effective against atypical bacteria such as mycoplasma and chlamydia. Macrolides are also used in some cases for S. pneumoniae and M. catarrhalis, but there is increasing bacterial resistance to these antibiotics. All but erythromycin are effective against H. influenzae. Macrolide-resistance rates doubled between 1995 and 1999 as more and more children were being treated with these antibiotics. Some research suggests these drugs may reduce the risk of a first heart attack in some patients by reducing inflammation in the blood vessels.
Extended-release (ER) azithromycin (Zmax) is the first anti-pneumonia antibiotic that can be given in a single dose. It is effective against Gram-positive, Gram-negative, and atypical bacteria. Studies have shown the results to be equal to those achieved with 7 days of levofloxacin or clarithromycin in patients with CAP. A single-dose antibiotic decreases the likelihood that a patient will stop taking the antibiotic early, which rapidly contributes to the development of drug-resistant bacteria.
Tetracyclines
Tetracyclines inhibit the growth of bacteria. They include doxycycline, tetracycline, and minocycline. They can be effective against S. pneumoniae and M. catarrhalis, but bacteria that are resistant to penicillin are also often resistant to doxycycline. The side effects of tetracyclines include:
- Burning in the throat
- Skin reactions to sunlight
- Tooth discoloration (which prevents use of these drugs in pregnant women and children)
Aminoglycosides
Aminoglycosides (gentamicin, tobramycin, and amikacin) are given by injection for very serious bacterial infections. Some are available in inhaled forms. Others can be applied in a solution directly to mucus membranes, skin, or body cavities. They can have very serious side effects, including:
- Balance problems
- Hearing damage
- Kidney damage
Lincosamides
Lincosamides prevent bacteria from reproducing. The only member of this group in clinical use is clindamycin (Cleocin). This antibiotic is useful against S. pneumoniae and S. aureus, but not against H. influenzae.
Glycopeptides
Glycopeptides (vancomycin, teicoplanin) are used for Staphylococcus aureu s infections that have become resistant to standard antibiotics. The drug must be given intravenously for pneumonia and other infections beyond the intestinal tract. The latest generation of glycopeptides, a derivative of vancomycin, is called telavancin. In studies of hospital-acquired pneumonia, it has shown promise for the treatment of Gram-positive pneumonia.
Trimethoprim-Sulfamethoxazole
Trimethoprim-sulfamethoxazole (Bactrim, Cotrim, and Septra) is less expensive than amoxicillin. It is particularly useful for adults with mild bacterial upper respiratory infections who are allergic to penicillin. The drug is no longer effective against certain streptococcal strains. It should not be used in patients whose infections occur after dental work, or in people who are allergic to sulfa drugs. Allergic reactions can be very serious.
Oxazolidinone
Linezolid (Zyvox) is the first antibacterial drug in a new class of man-made antibiotics called oxazolidinones. It has been shown to work against certain aerobic Gram-positive bacteria.
Another drug, tigecycline (Tygacil) is now approved for community-acquired bacterial pneumonia. It works against most gram-positive organisms including MRSA.
Other Medications
Inhaled polymyxin, a drug used in cystic fibrosis patients, is showing some effectiveness against pneumonia caused by multidrug-resistant Gram-negative bacteria, including pseudomonas and klebsiella.
Corticosteroid use in patients with pneumonia is also under study. Corticosteroids impact the immune system, carbohydrate and protein metabolism, electrolyte balance, and stress response. They may help to speed recovery and resolve symptoms, but more research is necessary to suggest recommendations for populations.
Surgery
Although most patients with pneumonia do not need invasive therapy, it may be necessary in patients with abscesses, empyema, or certain other complications.
Chest Tubes
Chest tubes are used to drain infected pleural fluid. Tubes are not typically required for pneumonia or abscesses. The tubes are inserted after the patient receives a local anesthetic. They remain in place for 2 - 4 days. They are removed in one quick movement. This can be very distressing, although some patients feel no discomfort. Complications of chest tubes include:
- Accidental injury to the lung
- Fluid build-up within the lung if the pleural fluid is removed too rapidly
- Infection
- Perforation of the diaphragm
Removing the chest tubes may cause the lung to collapse. In this case, a chest tube may be needed to inflate the lung.
Prevention
The best way to prevent serious respiratory infections such as pneumonia is to avoid sick people (if possible), and to practice good hygiene.
Good Hygiene and Preventing Transmission
Colds and flu are spread primarily from infected people who cough or sneeze. People commonly transmit a cold is when they shake hands. Research has found that washing hands frequently can prevent the spread of viral respiratory illnesses. Always wash your hands before eating and after going outside. Using ordinary soap is sufficient. Alcohol-based gels are also effective for everyday use, and may even kill cold viruses. If extreme hygiene is required, use alcohol-based rinses.
Antibacterial soaps add little protection, particularly against viruses. In fact, one study suggested that common liquid dishwashing soaps are up to 100 times more effective than antibacterial soaps in killing respiratory syncytial virus (RSV). Wiping surfaces with a solution that contains one part bleach to 10 parts water is very effective at killing viruses.
Changing Hospital Practices
Bacteria abound in hospitals and long-term care facilities. They are particularly able to cause disease in areas with the sickest patients, such as intensive care units. Health care facilities are changing many of their practices and educating doctors, nurses, and therapists about reducing the likelihood of transmitting bacteria.
Vaccines
Viral Influenza Vaccines (Flu Shot)
Description of Vaccines. Injected vaccines against the flu ("flu shots") use inactivated (not live) viruses. The nasal spray influenza vaccine uses an attenuated (greatly weakened) live flu virus. They are designed to provoke the immune system to attack antigens contained on the surface of the virus. Antigens are foreign molecules that the immune system recognizes and targets for attack.
Timing and Effectiveness of the Vaccine. Each year, scientists decide which viruses are likely to circulate during the upcoming flu season and make recommendations for updated seasonal vaccines. Ideally, people should get a flu shot every October or November. However, it may take longer for a full supply of the vaccine to reach certain locations. In such cases, high-risk groups should get vaccinated first.
The U.S. Centers for Disease Control and Prevention (CDC) Advisory Council recommends that all people ages 6 months and older, unless contraindicated, get a flu shot every year. These universal recommendations simplify earlier recommendations for specific high risk groups.
Older children and adults need only a single shot each year. However, children under age 9 may need two shots, given 1 month apart the first time they receive the flu vaccine or if they have not previously received two doses during a flu season.
Some people have a higher risk of the disease.
If supplies are limited, people in high risk groups, such as the following, should get a flu vaccine first:
- Young children
- Children over age 5 who have a higher risk for serious illness
- Household contacts, caregivers, or health care providers of children or adults with high-risk conditions
- Pregnant women (breastfeeding women may also receive the vaccine)
- People in long-term care facilities
- People who have chronic conditions such as asthma, diabetes, heart, lung or blood diseases
- People who receive long-term treatment with steroids for any condition
Pneumococcal Vaccines
The pneumococcal vaccine protects against S. pneumoniae bacteria, the most common cause of respiratory infections. There are two effective vaccines available:
- 23-valent polysaccharide vaccine (Pneumovax, Pnu-Immune) for certain older children and adults
- 13-valent conjugate vaccine (Prevnar or PCV13) for infants and children under 5 years of age
Experts are now recommending that more people, including healthy elderly people, receive the pneumococcal vaccine, particularly in light of the increase in antibiotic-resistant bacteria.
Pneumococcal Vaccine in Young Children. The Food and Drug Administration (FDA) recently approved the pneumococcal vaccine (Prevnar 13 or PCV13) for children 6 weeks to 5 years old for the prevention of pneumonia. It covers 13 types of pneumonia and replaces its earlier version PCV 7. Routine vaccination with the PCV7 vaccine began in 2000. The vaccine cut the rate of infant hospitalizations for pneumonia by a third between 1997 - 1999 and 2006. Possibly due to "herd immunity," pneumonia-related hospital admissions in adults ages 18 - 39 also dropped by more than 25%.
Many experts now recommend the new pneumococcal vaccine PCV 13 for all children up to age 5, and slightly older children with certain medical conditions. Healthy children who received the PCV 7 vaccine will complete their scheduled doses with the newer PCV 13. The pneumococcal conjugate vaccine has now been added to the Recommended Childhood Immunization Schedule. Studies are suggesting that it prevents common ear infections, as well as pneumonia in children.
The recommended schedule of immunization for Prevnar (PCV13) remains the same as the PCV 7 schedule in children: four doses, given at 2, 4, 6, and 12 - 15 months of age. Children starting their vaccinations between 12 and 23 months need only two doses. Those who are over 2 years old need only one dose. It is recommended that certain immunocompromised children be revaccinated once 5 years after the initial vaccination.
Pneumococcal Polysaccharide Vaccine in Older Children and Adults. The pneumococcal polysaccharide vaccine is proving to help reduce the rate of pneumonia in older children and adults. While it may be beneficial to patients with COPD, no significant improvements in outcomes have been seen in limited studies.
Still, pneumonia is declining among adults, which may be due to fewer infections transmitted from vaccinated young children.
The vaccine is recommended for:
- High-risk people age 2 or older (this includes people with heart disease, all lung diseases except asthma, kidney disease, alcoholism, diabetes, cirrhosis, and leaks of cerebrospinal fluid)
- Everyone ages 65 and older
- Adults aged 19 - 64 who have asthma or smoke should receive a single dose of PPV.
- Those with a nonworking spleen and those who have had their spleen removed should receive a second vaccine five years or more after the first dose
- Those with sickle cell disease
- People who live in nursing homes (extended-care facilities)
- Patients with autoimmune diseases, such as rheumatoid arthritis and lupus, although protection may not be as strong for these patients.
- Older people who have had transplant operations or those with kidney disease may require a revaccination after 6 years.
- People who live in any institution where there are people with chronic health problems
- People with conditions that weaken the immune system, such as cancer, HIV, organ transplantation, leukemia or lymphoma
- People who receive long-term medications that suppress the immune system (immunosuppressants), including steroids
- Alaskan natives and certain Native American populations
A single dose of the vaccine is given by injection. One dose works for most people. However, re-vaccination is recommended for people over age 65 who received their first dose before age 65 and more than 5 years ago. Other high-risk people, including those with a weakened immune system or spleen problems may also need a second dose after 5 years. You should speak with your doctor about specific reasons for vaccination and revaccination.
Because the vaccine does not contain live organisms, it is safe for pregnant women and people with immune problems. In fact, when the vaccine is given to pregnant women, it may actually protect their infants against certain respiratory infections.
Protection lasts for more than 6 years in most people, although it may wear off faster in elderly people than in younger adults. Anyone at risk for serious pneumonia should be revaccinated 5 years after the first dose, including those who were vaccinated before age 65. Later booster doses, however, are not recommended.
A PCV13 vaccine for adults is being studied but has not yet been approved.
Preventing Respiratory Syncytial Virus (RSV) Pneumonia in Children
Across the globe, RSV is the most common reason for acute lower respiratory infection in children under the age of 5. Parents often spread the infection to their baby. A simple way to help prevent RSV infection is to wash your hands often, especially before touching your baby. It is important to make sure that other people, especially caregivers, take precautions to avoid giving RSV to your baby. The following simple steps can help protect your baby:
- Insist that others wash their hands with warm water and soap before touching your baby.
- Have others avoid contact with the baby if they have a cold or fever. It may be helpful for them to wear a mask.
- Be aware that kissing the baby can spread RSV infection.
- Try to keep young children away from your baby. RSV is very common among young children, and easily spreads from child to child.
- Do not smoke inside your house, car, or anywhere near your baby. Exposure to tobacco smoke increases the risk of RSV illness.
- Have children above 6 months of age and all household members immunized against influenza.
Prevention of RSV. Two medications have been approved for protecting high-risk children against RSV pneumonia:
- Palivizumab (Synagis) is known as a monoclonal antibody, a genetically engineered antibody that targets the RSV virus. It is given by an injection into the muscle. Early studies of motavizumab, another monoclonal antibody in development, also show that it protects against RSV.
- RSV immune globulin (RespiGam) is made up of antibodies to RSV that are taken from the blood of healthy infants. RespiGam is given as a shot.
The American Academy of Pediatrics updated its recommendations for high risk infants and children, and appropriate RSV prophylaxis in 2009. The updated recommendations reflect the Centers for Disease Control and Prevention (CDC) seasonality and regional guidelines, newer dosing schedules, and a narrower definition of at-risk children.
Statin Use in Adults
In a review of research evidence, statin use was shown to improve the outcome in patients with bacterial pneumonia. Researchers, however, stress the need for additional controlled research.
Resources
- www.lungusa.org -- American Lung Association
- www3.niaid.nih.gov -- National Institute of Allergy and Infectious Diseases
- www.cdc.gov -- Centers for Disease Control and Prevention
References
Attridge RT, Frei CR. Health care-associated pneumonia: an evidence-based review. Am J Med. 2011;124(8):689-97. Review.
Baum SG. Mycoplasma pneumoniae and atypical pneumonia. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, Pa: Elsevier Churchill Livingstone; 2009:chap 184.
Bradley JS, Byington CL, Shah SS, et al. Executive summary: the management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):617-30.
Butt S, Swiatlo E. Treatment of community-acquired pneumonia in an ambulatory setting. Am J Med. 2011;124(4):297-300. Review.
Centers for Disease Control and Prevention. Recommended adult immunization schedule—United States, 2012. MMWR 2012;61(4).
Centers for Disease Control and Prevention. Recommended Immunization Schedules for Persons Aged 0 Through 18 Years --United States, 2012, MMWR 2012;61(05);1-4.
Chen Y, Li K, Pu H, Wu T. Corticosteroids for pneumonia. Cochrane Database Syst Rev. 2011;(3). Review.
Chopra V, Flanders SA. Does statin use improve pneumonia outcomes? Chest. 2009;136(5):1381-8.
Committee on Infectious Diseases. Modified recommendations for use of palivizumab for prevention of respiratory syncytial virus infections. Pediatrics. 2009;124:1694-1701.
Donowitz R. Acute Pneumonia. In: Mandell GL, Bennett JE, Dolin R, eds. Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, Pa: Elsevier Churchill Livingstone; 2009:chap 64.
Ebell MH. Clinical diagnosis of pneumonia in children. Am Fam Physician. 2010;82(2):192-3. Review.
Grant GB, Campbell H, Dowell SF, et al; World Health Organization Department of Child and Adolescent Health and Development. Recommendations for treatment of childhood non-severe pneumonia. Lancet Infect Dis. 2009(3):185-96
Kabra SK, Lodha R, Pandey RM. Antibiotics for community-acquired pneumonia in children. Cochrane Database Syst Rev. 2010;(3). Review.
Knol W, van Marum RJ, Jansen PA, Souverein PC, Schobben AF, Egberts AC. Antipsychotic drug use and risk of pneumonia in elderly people. J Am Geriatr Soc. 2008;56:661-666.
Lassi ZS, Haider BA, Bhutta ZA. Zinc supplementation for the prevention of pneumonia in children aged 2 months to 59 months. Cochrane Database Syst Rev. 2010;12. Review.
Lee JS, Primack BA, Mor MK, et al. Processes of care and outcomes for community-acquired pneumonia. Am J Med. 2011;124(12):1175.
Lim WS, Baudouin SV, George RC, et al; Pneumonia Guidelines Committee of the BTS Standards of Care Committee. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009; 64:1-55
Limper AH. Overview of Pneumonia. In: Goldman L, Ausiello D. Goldman: Cecil Medicine. Philadelphia, Pa: Saunders; 2007:chap 97.
Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44:S27-S72.
Meissner HC, Long SS. American Academy of Pediatrics Committee on Infectious Diseases and Committee on Fetus and Newborn. Revised indications for the use of palivizumab and respiratory syncytial virus immune globulin intravenous for the prevention of respiratory syncytial virus infections. Pediatrics. 2003;112:1447-1452.
Mills K, Graham AC, Winslow BT, Springer KL. Treatment of nursing home-acquired pneumonia. Am Fam Physician. 2009;79(11):976-82. Review.
Nair H, Nokes DJ, Gessner, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375(9725):1545-55. Review.
Niederman M. In the clinic. Community-acquired pneumonia. Ann Intern Med. 2009;151(7):ITC4-2-ITC4-14. Review. Erratum in: Ann Intern Med. 2009;151(11):827.
Pugh R, Grant C, Cooke RP, Dempsey G. Short-course versus prolonged-course antibiotic therapy for hospital-acquired pneumonia in critically ill adults. Cochrane Database Syst Rev. 2011;(10). Review.
Ruuskanen O, Lahti E, Jennings LC, Murdoch DR. Viral pneumonia. Lancet. 2011;377(9773):1264-75. Review.
Sing S, Amin AV, Loke YK. Long-term use of inhaled corticosteroids and the risk of pneumonia in chronic obstructive pulmonary disease: A meta-analysis. Arch Intern Med. 2009;169:219-229.
Venditti M, Falcone M, Corrao S, Licata G, Serra P. Outcomes of patients hospitalized with community-acquired, health-care associated, and hospital-acquired pneumonia. Ann Intern Med. 2009;150:19-26.
|
Review Date:
4/26/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |















